CULTURAL SAFETY AND QUALITY
Cultural safety and quality: Are evidence and strengths based on best practice approaches to Aboriginal and or Torres Strait Islander healthcare.
The descriptors in module 2 Safety and Quality:
Descriptor 1: Population health
- Demographics - data relating to the populations and particular groups within it
- Morbidity - condition of being diseased
Descriptor 2: Social and cultural determinants
Descriptor 3: Safer healthcare
Descriptor 4: Healthcare models
A strategy for embedding cultural safety into the health system.
The National Scheme's Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy 2020-2025 has been developed through the Australian Health Practitioner Regulation Agency (AHPRA). The Strategy has been developed from the knowledges of Aboriginal and Torres Strait Islander health experts, regulators and health organisations committed to embedding cultural safety into the health system will be released tomorrow.
AHPRA states that the Strategy is endorsed by 43 organisations, academics and individuals, including the entities who set the education standards for the 183,000 students who are studying to become registered health practitioners and the regulators of Australia’s 750,000 registered practitioners.
Read or download the National Scheme's Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy
The Overview of Aboriginal and Torres Strait Islander health status (Overview) aims to provide a comprehensive summary of the most recent indicators of the health and current health status of Australia’s Aboriginal and Torres Strait Islander people. The initial sections of the Overview provide information about the context of Aboriginal and Torres Strait Islander health, population, and various measures of population health status. The remaining sections are about selected health conditions and risk and protective factors that contribute to the overall health of Aboriginal and Torres Strait Islander people. These sections comprise an introduction and evidence of the extent of the condition or risk/protective factor.
Descriptor 1: Population Health
Introduction
You will cover the following as part of the Safety and Quality cultural capability:
- Population Health
- Social and cultural determinants
This topic aims to develop students’ knowledge of the current demographic and contemporary health status for Australia’s First Peoples.
Learning Outcomes
Upon the completion of this topic you should be able to identify current demographic, health indicators and statistical trends for Australia’s First Peoples.
Content
What is population health?
Population health refers to all organised measures to prevent disease, promote health and prolong life among the population as a whole (WHO, 2016a). The aim of a population health approach is to provide conditions in which people can be healthy, and focus on entire populations, not individual disease (WHO, 2016a).
Change in health outcomes must involve actions directed at strengthening the skills and capabilities of individuals as well as action directed towards social, environmental and economic conditions, known as determinants of health discussed in topic 2.2 (WHO, 1986).
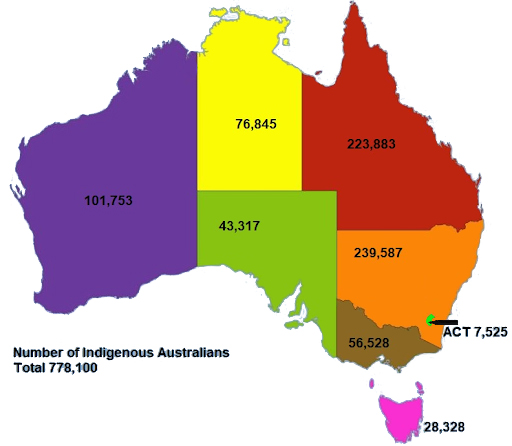
Distribution of First Peoples in Australia
It is often mistakenly believed Australia’s First Peoples live in remote or isolated areas. However, the majority of First Peoples (81%) live in major cities and non-remote areas with 19% living in remote or very remote locations.
Geographic distribution (ABS, 2016)(ABS, 2014, ABS, 2018).
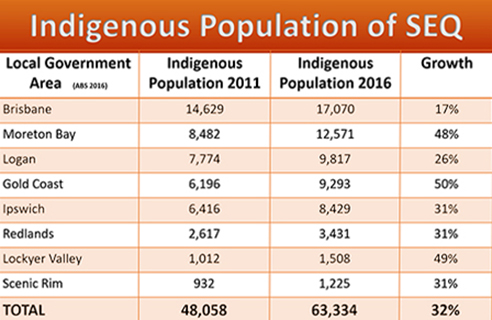
First Peoples Populations in South East Queensland
There has been a significant increase in the First Peoples population of SEQ, in the past 5 years, the Gold Coast region has the fastest growing First Peoples population (ABS 2016). Understanding who comprises the community in which you live and work aids in your understanding of the diversity you are likely to encounter in the workplace.
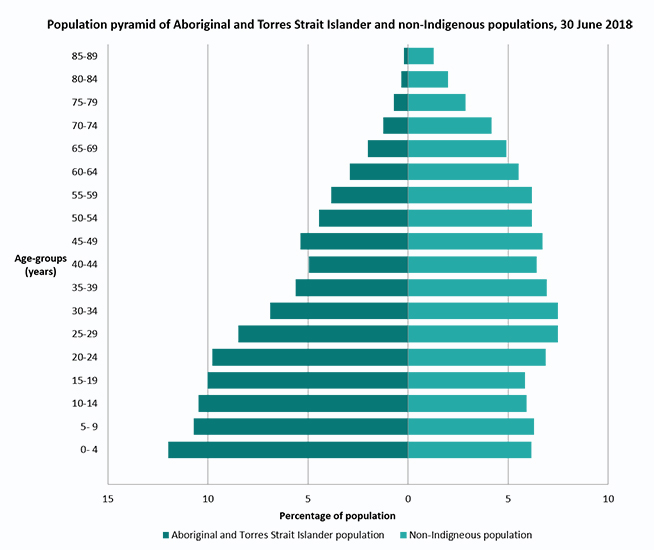
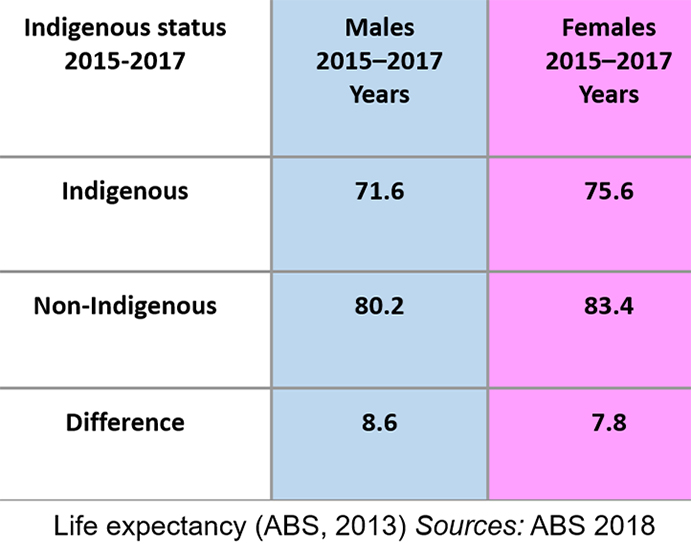
Age Group Comparison
Note: Excludes 90 years and older age-group.
Sources: Derived from ABS, 2018, ABS, 2014
Causes of Morbidity
Morbidity refers to levels of heath/disease in a population or group (ABS, 2014; AIHW, 2015).
The top 4 causes of morbidity include Circulatory Disease, Cancer, Diabetes, and Respiratory Disease.
National Agreement for Closing The Gap
Coalition of Peaks
What makes us live longer? Keeping culture central
Strong connection to culture and positive identity as First Peoples is highly protective against some of the noted health challenges within community. Consequently, it is important to keep a person’s culture and positive identity at the forefront of healthcare practice, ensuring respect for both is always maintained. Consider how you might demonstrate respect for these aspects of wellbeing in your own practice.
Aboriginal and Torres Strait Islander Health Performance Framework
Descriptor 2: Social and Cultural Determinants
Introduction
This topic introduces students to the concepts of the social and cultural determinants of health.
Learning Outcome
Upon the completion of this topic you should be able to identify, differentiate and compare the strengths and challenges in delivering healthcare with respect to the social and cultural determinants of health.
Content
The social determinants of health are the conditions in which people are born, grow, work, live and age. They are the wider set of forces and systems shaping the conditions of life. These include economic, policies, systems, development agendas, social norms, social policies and political systems (WHO, 2016).
Promoting a Social and Cultural Determinants Approach to Aboriginal and Torres Strait Islander Affairs states that cultural determinants of health "originate from and promote a strength based perspective, acknowledging that stronger connections to culture and country build stronger individual and collective identities, a sense of self-esteem, resilience, and improved outcomes across the social determinants of health including education, economic stability and community safety" (Promoting a Social and Cultural Determinants Approach to Aboriginal and Torres Strait Islander Affairs, Lowitja Institute, 2014, n.p).
The National Aboriginal and Torres Strait Islander Health Plan 2013-2023 was developed by the Council of Australian Governments (COAG). The Plan identifies as crucial, an Australian health system that is free of racism and inequality and all Aboriginal and Torres Strait Islander people have access to health services that are effective, high quality, appropriate and affordable. Together with strategies to address social inequalities and determinants of health, this provides the necessary platform to realise health equality by 2031 (Australian Government. (2013). National Aboriginal and Torres Strait Islander Health Plan 2013-2023 (Canberra: Department of Health).
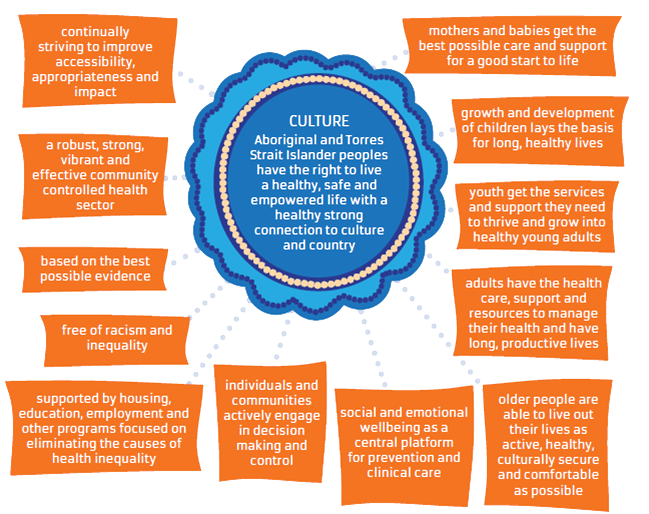
(Figure Reference: Australian Government. (2013). National Aboriginal and Torres Strait Islander Health Plan 2013-2023. (Canberra: Department of Health).
This image further highlights the importance of the central positioning of culture for First Peoples wellbeing and healthcare practice, linking it to practical applications within service provision. Consider how you may apply these strategies within your own professional practice.
To understand these health disparities requires understanding of the factors and processes outside traditional domains of health. These are the structures of society and social conditions in which people grow, live, work and age (Zubrick et al., 2014).
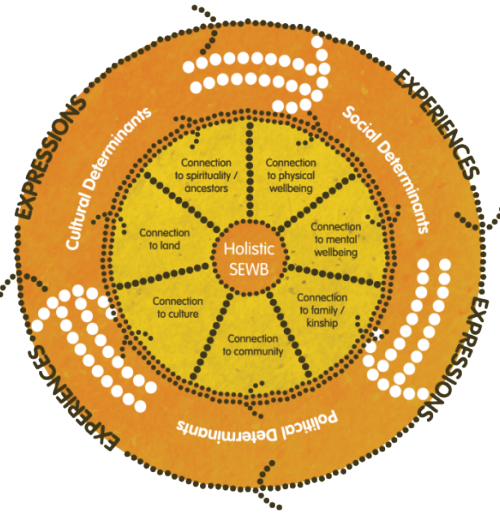
Image source: Gee, G., Dudgeon, P., Schultz, C., Hart, A., Kelly, K. (2014). Aboriginal and Torres Strait Islander Social and Emotional Wellbeing. In P. Dudgeon, P. Milroy, Walker, R. (Eds.). Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice (pp. 55 – 68). ACT, Australia: Commonwealth of Australia. Artwork by Tristan Schultz.
Determinant: a factor which decisively affects the nature or outcome of something.
Cultural Determinants
Culture as a determinant of health, includes building on strengths of First Peoples: protection/ promotion of aspects of long-standing (traditional) knowledge, beliefs and practices that are shared via relationships to people (i.e. family and kinship roles communities) and relationships to Country (ancestral origins and connections) e.g. Birthing on Country; using local flora or oil extracts to treat ailments.
Social Determinants
Social determinants of health include education, employment, the environment and racism. They all have the ability to influence holistic health and wellbeing for First Peoples.
Lowitja Institute. (2014). Cultural determinants of Aboriginal and Torres Strait Islander health roundtable.
Political Determinants
Political determinants have the ability to effect health, as evidenced by the historical policies for first peoples as discussed in the Respect Capability. Political determinants shape the lives of all people hence, still influence health for First Peoples today. For example Northern Territory Intervention.
National Aboriginal and Torres Strait Islander Health Plan 2013-2023
Read how the cultural determinants of health play a central role in protecting First Peoples wellness. Consider how clinical practices can be made culturally safer.
Descriptor 3: Safer Healthcare
Introduction
This topic develops students’ ability to identify considerations for providing culturally safer care for Aboriginal and Torres Strait Islander individuals, families and communities.
Learning Outcome
Upon the completion of this topic you should be able to identify the main principles/elements/practices for providing culturally safer care for Aboriginal and Torres Strait Islander individuals, families and communities.
Health Service Access
Non-Indigenous health services are the largest source of health provision to First Peoples despite the misconception that First Peoples predominately access Aboriginal Community Controlled Health Services for their health care needs (Larkins et al., 2006). To improve First People's health, we need to improve access to health care services for First Peoples and communities.
Access does not only include physical access, it also includes:
- Services that are culturally safe – free from racism;
- Services that are economically accessible and affordable, based on the principle of equity; and
- Health information is culturally responsive and accessible.
Evidence shows that First Peoples are more likely to access health services where service providers communicate respectfully, have some understanding of culture and build good relationships (Durey, Thompson & Wood, 2011; Shahid, Finn, & Thompson, 2009).
Developing a therapeutic relationship between health professional and client may be the cornerstone to improving individual health outcomes for First Peoples, this includes:
- Remaining flexible with their time;
- Allowing opportunities for the client to talk or tell their story; and
- To actively listen.
Active listening to the client’s story, will assist the health professional in building rapport and trust which play a considerable role in health outcomes for the client.
It is important when considering clinical care for First Peoples, that the individual is considered holistically, using a social and cultural determinants of health lens. Watch this short video of two Griffith University medical students who share their professional experience on Palm Island.
It is important when considering clinical care for First Peoples, that the individual is considered holistically, using a social and cultural determinants of health lens. Watch this short video of two Griffith University medical students who share their professional experience on Palm Island.
The following is what students can encounter in the clinical context that could influence health outcomes for First Peoples:
- Identity
- Chronic disease with co-morbidity e.g. uncontrolled hypertension and diabetes
- Social/ Emotional determinants e.g. education, environment
- Cultural determinants e.g. connection to land, kinship
- Political determinants e.g. government policy
Descriptor 4: Healthcare Models
Introduction
This descriptor introduces students to the dominant western cultural paradigm of the Australian healthcare system. It develops the students’ ability to understand the characteristics of the mainstream health care system.
Learning Outcome
Upon the completion of this topic you should be able to define Australia's dominant western cultural paradigm and discuss how this influences the contemporary health system.
Content
How we make sense of our values and beliefs about health care comes from various different frameworks of health. Different models of health have informed the way in which medicine and healthcare has evolved.
What is health? Health is defined in several ways. Consider the following definitions of health:
The World Health Organisations’ Model of Health (WHO, 1946): A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.
First Peoples Model of Health:
“Aboriginal health” means not just the physical well-being of an individual but refers to the social, emotional and cultural well-being of the whole Community in which each individual is able to achieve their full potential as a human being, thereby bringing about the total well-being of their Community. It is a whole-of-life view and includes the cyclical concept of life-death-life (National Aboriginal Health Strategy, 1989).
Social & Emotional Wellbeing:
Social and emotional wellbeing is a multidimensional concept that encapsulates mental health, in addition to connection to country, culture, spirituality, ancestry, family and community. Culture is placed at the centre of this definition of health, and recognises the impact that social, cultural, historical and political determinants of health (Dudgeon et al., 2014).
The Biomedical Model of Health:
This is a narrow view of health concerned only with physical changes to the body. In this view, Western medicine aims to restore balance for the body to function (Taylor & Guerin, 2014).
Health care services that make up the healthcare system in Australia are dominated by tertiary hospitals that largely treat patients at the end stages of disease using principles of Western medicine. What may be the implications of treating patients who share different views of health than the dominant biomedical model?
NOW TAKE THE QUIZ FOR CULTURAL SAFETY AND QUALITY...
ReferencesAustralian Bureau of Statistics (ABS). (2014). Australian Aboriginal and Torres Strait Islander Health Survey: updated results, 2012–13. ABS cat. no. 4727.0.55.006. Canberra: ABS. Australian Bureau of Statistics (ABS). (2016). Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. Cat. No. 3238.0.55.001. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001 Australian Bureau of Statistics (ABS). (2018). Life Tables for Aboriginal and Torres Strait Islander Australians, 2015-2017. Cat. No. 3302.0.55.003. Retrieved from this page. Australian Indigenous HealthInfoNet (2019) Overview of Aboriginal and Torres Strait Islander health status, 2018. Perth, WA: Australian Indigenous HealthInfoNet Australian Institute of Health and Welfare (AIHW). (2015). The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples. Cat. no. IHW 147. Canberra: AIHW. Nash, D. et al. (2011). Population health: creating a culture of wellness. [online version]. Retrieved from http://librarycatalogue.griffith.edu.au/record=b2182154 Lowitja Institute. (2014). Cultural determinants of Aboriginal and Torres Strait Islander health roundtable. Available from: http://www.lowitja.org.au/cultural-determinants-roundtable#sthash.HEofHQ61.dpuf World Health Organisation (WHO). (2016a). Glossary, Public Health. Retrieved from http://www.who.int/hia/about/glos/en/index2.html World Health Organisation (WHO). (2016b). Mortality. Retrieved from http://www.who.int/topics/mortality/en/ World Health Organisation (WHO). (1986). Ottawa Charter for Health Promotion. Geneva, Switzerland: WHO Australian Government. (2013). National Aboriginal and Torres Strait Islander Health Plan 2013 - 2023. Canberra: Commonwealth of Australia Lowitja Institute. (2014). Cultural determinants of Aboriginal and Torres Strait Islander health roundtable. Available from: http://www.lowitja.org.au/cultural-determinants-roundtable#sthash.HEofHQ61.dpuf World Health Organisation (WHO). (2016a). Glossary, Public Health. Retrieved from http://www.who.int/hia/about/glos/en/index2.html WHO. (2016b). Mortality. Retrieved from http://www.who.int/topics/mortality/en/ WHO. (1986). Ottawa Charter for Health Promotion. Geneva, Switzerland: WHO Australian Government. (2013). National Aboriginal and Torres Strait Islander Health Plan 2013 - 2023. Canberra: Commonwealth of Australia Lowitja Institute. (2014). Cultural determinants of Aboriginal and Torres Strait Islander health roundtable. Available from: http://www.lowitja.org.au/cultural-determinants-roundtable#sthash.HEofHQ61.dpuf World Health Organisation (WHO). (2016a). Glossary, Public Health. Retrieved from http://www.who.int/healthpromotion/about/HPG/en/ Zubrick, S.R., Dudgeon,P., Gee, G., Glaskin,B., Kelly, K., et al (2010). Social Determinants of Aboriginal and Torres Strait Islander Social and Emotional Wellbeing In N. Purdie, P. Dudgeon, & R. Walker (Eds.), Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Australia: Department of Health and Ageing Durey, A., Thompson, S.C. & Wood, M. (2011). ‘Time to bring down the twin towers in poor Aboriginal hospital care: addressing institutionalised racism and misunderstandings in communication’, Internal Medicine Journal, vol. 42, no. 1, pp. 17-22. Foley & Houston. (2014).Closing the gap by increasing access to clinical dietetic services for urban Aboriginal and Torres Strait Islander people. Nutrition & Dietetics (71) 216 – 222. Gale, J. (2012). A practical guide to health behaviour change: using the HCA approach. Australia: Health Change Australia. Larkins, S. L., Geia, L. K., & Panaretto, K. S. (2006). Consultations in general practice and at an Aboriginal community controlled health service: do they differ? Rural and Remote Health, 6(560) Larkins, S. L., Geia, L. K., & Panaretto, K. S. (2006). Consultations in general practice and at an Aboriginal community controlled health service: do they differ? Rural and Remote Health, 6(560) Shahid, S., Finn, L., & Thompson, S.C. (2009). ‘Barriers to participation of Aboriginal people in cancer care: communication in the hospital setting’. Medical Journal of Australia, vol. 190, pp. 574-579. |